Understanding Epilepsy: A Comprehensive Guide
Epilepsy is a neurological condition that affects over 50 million people worldwide, including around 6 million in Europe. It impacts individuals of all ages, with a particular prevalence among children, adolescents, and the elderly. This blog post draws from detailed educational materials on epilepsy awareness to provide an in-depth overview. We’ll explore what epilepsy is, its causes, types of seizures, diagnosis, treatment options, associated risks, and practical advice for living with the condition. Whether you’re someone living with epilepsy, a caregiver, or simply seeking knowledge, this guide aims to inform and empower.
What is Epilepsy?
Epilepsy is defined as a brain disorder characterized by recurrent seizures that originate in the brain. Not every seizure means epilepsy—anyone can have a one-off seizure due to factors like high fever or injury. A diagnosis typically follows repeated seizures, confirmed by a specialist, often with expertise in epilepsy as recommended by the National Institute for Health and Care Excellence (NICE).
Key principles include:
- Seizures result from abnormal electrical activity in the brain, disrupting normal functions like movement, sensation, awareness, or behavior.
- It can start at any age and may be lifelong, though some forms resolve over time.
- Most people with epilepsy can control seizures through management, leading to normal daily lives with some precautions.
- Diagnosis should involve patient participation, considering cultural needs, and providing accessible information.
NICE guidelines (CG137 for diagnosis and management, QS27 for children/young people, QS26 for adults) emphasize tailored care, annual reviews, and discussions on risks like sudden unexpected death in epilepsy (SUDEP) before seizures occur.
Anatomy and Physiology of Epilepsy
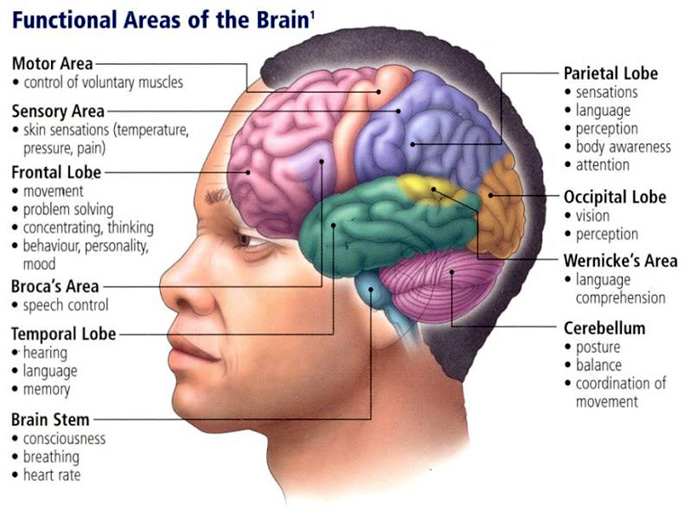
Understanding epilepsy starts with the brain’s structure. The human brain has a highly developed outer layer called the cerebral cortex, divided into lobes with specific functions:
- Frontal lobe: Handles concentration, memory, decision-making, emotional responses, impulse control, language, voluntary movement, and consciousness.
- Parietal lobe: Manages touch, temperature, pain perception, and spatial awareness.
- Temporal lobe: Involved in hearing, memory, language interpretation, visual perceptions, and behavior. The hippocampus here is prone to abnormalities causing seizures.
- Occipital lobe: Processes vision.
Epilepsy / Physical consequences / Consequences | Brain-injury …
Seizures depend on where they start and spread, causing changes in sensation, awareness, behaviour, or movement. At the cellular level, brain cells communicate via neurotransmitters: excitatory ones (like glutamate) promote activity, while inhibitory ones (like GABA) slow it down. An imbalance—too much excitation or too little inhibition—can lead to uncontrolled signalling and seizures.
The brain’s motor areas are sensitive to triggers like low oxygen, metabolic changes, or infections. Abnormalities like hippocampal sclerosis or focal cortical dysplasia can propagate seizures, leading to symptoms such as abdominal pain (temporal lobe), visual hallucinations (occipital), auditory issues, or Jacksonian marches (progressive muscle twitching on one side).
Prolonged or recurrent seizures can damage neurons, especially if lasting over 20-30 minutes. Seizures often have phases: an aura (warning like unusual smells), the ictus (seizure itself), and postictal state (recovery).
Causes of Epilepsy
Epilepsy can be symptomatic (known cause like brain injury or infection), idiopathic (no identifiable cause), or cryptogenic (suspected but unknown cause). High-risk groups include infants, where incidence is highest, often due to epileptic spasms or febrile seizures. Genetic factors, molecular errors, and neuroimaging reveal brain abnormalities.
Triggers include decreased oxygen, metabolic imbalances, infections, or sensitivities like photosensitivity in juvenile myoclonic epilepsy (JME). Neuroinflammation plays a role in focal epilepsies like temporal lobe epilepsy with hippocampal sclerosis.
Seizure Classifications
Seizures are classified by origin and symptoms. Here’s a breakdown:
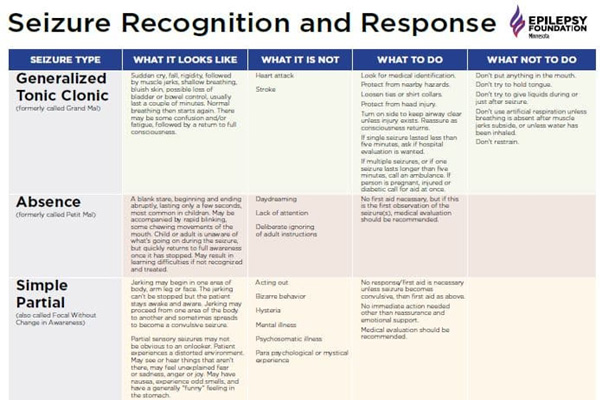
Focal (Partial) Seizures
Start in one brain area, potentially spreading. Symptoms vary by location:
- Simple partial: No loss of awareness; may involve twitching, tingling, or sensory changes.
- Complex partial: Altered awareness; often in temporal lobe, causing confusion, lip-smacking, or emotional changes.
- With secondary generalization: Spreads to both sides, becoming tonic-clonic.
Seizure Recognition and Response Chart – Epilepsy Foundation of …
Generalised Seizures
Affect both brain sides from the start:
- Tonic-clonic (grand mal): Stiffening, jerking, loss of consciousness; may include cries, falls, or post-seizure fatigue.
- Absence (petit mal): Brief loss of awareness, staring; common in children, may interfere with learning.
- Atypical absence: Slower onset, longer duration, possible confusion.
- Myoclonic: Sudden jerks, often in arms/shoulders; JME involves photosensitivity.
- Atonic (drop attacks): Sudden limpness, falls.
- Tonic: Stiffening without jerking.
Other types include:
- Status epilepticus: Prolonged (>5 minutes) or multiple seizures without recovery.
- Dravet syndrome: Severe infantile seizures with developmental issues.
- Catamenial: Linked to menstrual cycle hormone changes.
Keeping a seizure diary (noting date, time, triggers, symptoms) aids diagnosis and management.
Diagnosis
Diagnosis requires a specialist, often involving eyewitness accounts. NICE stresses urgent assessment for suspected seizures. For children/young people, see a specialist within 2 weeks; adults within 2 weeks for first seizure.
Clinical observations include neurological exams and considering neuroinflammation in focal epilepsies. Tools:
- EEG: Records brain activity; may provoke with lights/hyperventilation.
- MRI/CT: Detect structural issues.
- PET/SPECT: Analyze function/blood flow.
- Blood tests/lumbar puncture: Rule out infections/electrolyte issues.
For learning disabilities, involve multi-professional teams and tools like the Epilepsy Outcome Scale. Misdiagnosis occurs in 5-30% of cases, so monitoring is key.
Treatment Options
Treatment aims for seizure control with minimal side effects.
Medication
Anti-epileptic drugs (AEDs) control 70% of cases. Examples by seizure type:
- Absence: Ethosuximide, lamotrigine, sodium valproate.
- Tonic-clonic: Carbamazepine, lamotrigine, sodium valproate.
- Focal: Carbamazepine, gabapentin, levetiracetam.
- Myoclonic: Clonazepam, sodium valproate.
Buccal midazolam treats prolonged seizures (status epilepticus). Side effects include drowsiness, dizziness; tolerance may develop.
For children, AEDs are first-line; ketogenic diets (high-fat, low-carb) reduce seizures in 50-60% of resistant cases.
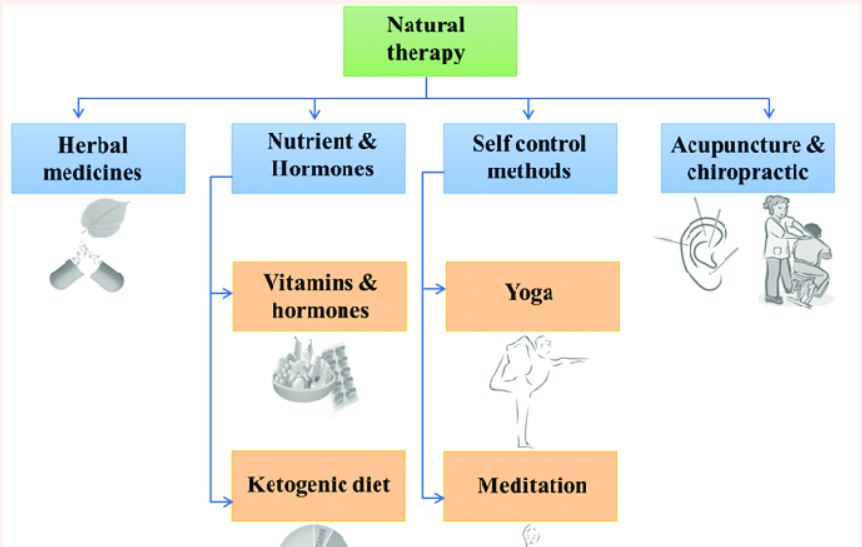
Natural epilepsy treatment options. | Download Scientific Diagram
Invasive Treatments
Surgery for drug-resistant cases: Removes seizure focus (e.g., lesionectomy, lobectomy). Success depends on pre-surgical evaluation (EEG, MRI, neuropsych testing). Vagus nerve stimulation reduces seizures by 50% in some.
Associated Risks
- SUDEP: Sudden death in uncontrolled epilepsy; minimize by optimizing control and monitoring nocturnal seizures.
- Psychiatric Disorders: Higher anxiety, depression; multidisciplinary care needed.
- Cognitive Issues in Children: 20% have intellectual disabilities; behavioral problems common.
- Pregnancy: Increased seizure risk; AEDs may cause fetal malformations (4-6% vs. 2-3% general). Preconception counseling, folic acid, genetic testing advised. Fertility may be impacted by syndromes like polycystic ovaries.
Living with Epilepsy
People with epilepsy lead full lives with precautions.
Home Safety
- Fix floor coverings, use sturdy furniture.
- Install smoke alarms, fireguards.
- In kitchen: Use cooker guards, microwaves.
- Bathroom: Prefer showers; supervise children.
- Bedroom: Avoid smoking in bed; consider alarms.
Higher risks for severe/unpredictable seizures or comorbidities like dementia.
Daily Life
- Alcohol/Caffeine: Moderate; alcohol reduces AED effectiveness.
- Computers: Safe; take breaks.
- Sports: Most okay; avoid high-risk like scuba diving. Supervise swimming.
- Driving: Must be seizure-free (1 year for cars); notify DVLA.
- Benefits: Check PIP/DLA eligibility.
- Cinema/Discos: Safe unless photosensitive; avoid strobes.
For children: Supervise water/sports; inform schools for SEN support.
Conclusion
Epilepsy is manageable with proper diagnosis, treatment, and lifestyle adjustments. Awareness reduces stigma and improves outcomes. Consult specialists and resources like Epilepsy Action (epilepsy.org.uk) or SUDEP Action (sudep.org) for support. If you or a loved one has epilepsy, focus on control and safety—knowledge is key to thriving.
